Toni's story

Toni Lynch
Interim Chief Nurse
(until October 2020)
“At one meeting we had the thought we might lose some of our team. That was hard. We are not the military.”

“I was passing a matron in the corridor one day when she called me over. She was older and wearing scrubs and on her way to work in intensive care. I said, 'Look at you, in your scrubs!' I was trying to be light hearted. She said: ‘I last worked in intensive care in 1995. I’m about to do my first shift.’
She was scared. It was not lost on me how scared she was. We have 6,000 nurses in post and we needed 500 extra in critical care. I thought they would all be clambering to get in. That moment brought home how much I was asking. You plan it, and then you see the reality. Like her, I last worked in intensive care in 1995. She was being absolutely courageous.
At one meeting of senior nurses early on, when the enormity of what we were facing hit us, we had the thought that we might lose some of our team. That was hard. We have lost staff in the past to terrorism. But this was on a different scale. We are not the military.
We knew this was going to be big when the High Consequence Infectious Diseases unit (HCID) stopped taking COVID-19 patients in February. There were too many, they were overwhelmed, so they had to be treated in general wards.
“We needed 500 extra nurses for critical care. I’d never done that. No one had. We had to condense training into two days.”
There was one ward that was mothballed and we needed 60 nurses to open it as a COVID-19 ward. We found them in 48 hours from across the Trust - that was the easy bit. People had stopped coming to A&E and the wards were growing quieter.
But 500 extra staff for critical care? I’d never done that before. No one had. We had to find people who had worked in ITU, assess their skills and identify who could be released. We had to condense a training and education package that normally takes 6 months into 2 days.

Critical care training was condensed into 2 days
Critical care training was condensed into 2 days
At first they spent a day in the simulation suite where we took them through inserting lines, infusion pumps, ventilators. Later it was half a day – we were under too much pressure. Then they worked as a supernumerary alongside a trained nurse for 2 days, asking questions.
It was the scale and speed that was the challenge. We were trying to do all this whilst also being personal.
Some nurses loved it and flourished. Others struggled. If they couldn’t cope psychologically, we supported them to come out and return to their old jobs. There were very few at that stage. But now more are saying if there is a second wave they wouldn’t want to go back because of what they saw in the first wave.
We have all seen death as nurses, but there were more deaths, on the wards as well as in critical care, and nurses found it difficult. Nurses are people. Like everybody else, they worry about their families, they are affected by what they read in the media.
“Nurses that flourished talked about the adrenaline rush, that this was what they trained for. This is our time, they said.”
Nursing is very a sociable profession. Nurses go to the pub after work or out for a picnic and share experiences. But under lockdown they lost the ability to socialise and their peer support networks went too. Some were also separated from their families if they were shielding.
Those that flourished talked about the adrenaline rush, that this was what they trained for. This is our time, they said. They loved the weekly NHS clap, they were inundated with donations of food and gifts. The NHS is often portrayed in a negative light and this was a sea change. But it had worn off by the beginning of June. By then exhaustion was kicking in.
Despite difficult conditions the Trust's survival rate was high
Despite difficult conditions the Trust's survival rate was high
Doubling critical care capacity meant halving the space – 4 beds where there had been 2. Nurses were working in cramped conditions and some became distressed as they struggled to maintain standards. I’m an A&E nurse and I said: 'You’re saving lives, that’s what matters.' But some found it difficult to reconcile. In fact, survival in our critical care unit was very high.
My biggest worry was ensuring there were enough staff. At one point we had 500 nurses off sick or self-isolating. But there was extraordinary goodwill. Admin staff volunteered to provide support on the wards. Later it became clear people were dying at home and we needed a team to go out into the community. Providing care to a COVID-19 patient in their home is completely different from on the ward. The nurses who volunteered, doing it virtually on their own, were really courageous.

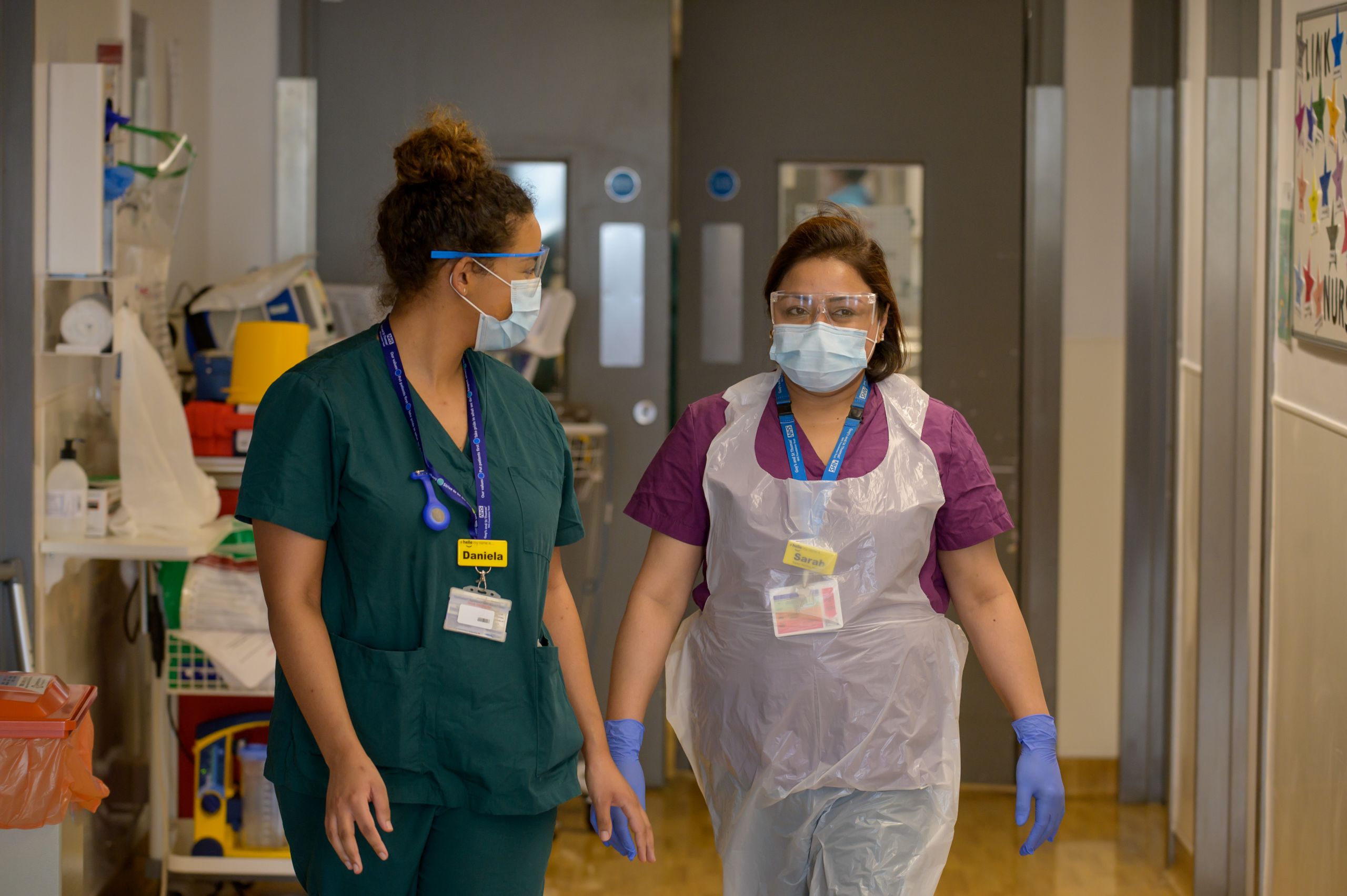
Community nurses visited patients' homes
Community nurses visited patients' homes
Early on we had a pod outside the hospital to provide testing and dental nurses did the swabbing. Then, when the Government abandoned testing, they moved to critical care to provide mouth care. Now they are testing people at home before they come in for elective treatment. They have been the most amazingly flexible group.
We have made mistakes. We started with a fixed rota in critical care because it was felt that was the only way to cope. But everyone has families and unpredictable lives and that doesn’t stop. Staff started to complain about the lack of flexibility. In the context of the pandemic we didn’t need that.
Staff checking the nursing rota
Staff checking the nursing rota
We doubled the critical care beds but we didn’t think to double the leadership. Staff complained matrons weren’t visible and the matrons felt upset. We had ward matrons who could have checked on staff. With hindsight we should have thought of that.
I live in Gloucester with my wife but the trains weren’t reliable so I had to stay in a hotel for three months. You end up living in a bubble – just working. My family were desperate to talk on Facetime but after a day of Zoom calls I had to say I just can’t do this. That was hard.
Some people found their place and others lost their sense of identity and purpose, and mourned it. Some created a new sense of purpose for themselves. The staff supermarket, the Wellbeing zones, the Rest and Recharge zones – there was so much ingenuity and imagination.
We are producing a guide in the next couple of weeks for a 2nd wave. How to staff beds, the impact of psychological factors, the impact of staff needing to go into self-isolation. We won’t want to switch off elective work next time. There is a lot to plan.”

Read more stories

